What do you think of this article?
By Dr. David Woo - Published on October 16, 2023
Last updated on January 6, 2025
Published: October 16, 2023 Updated: September 11, 2024
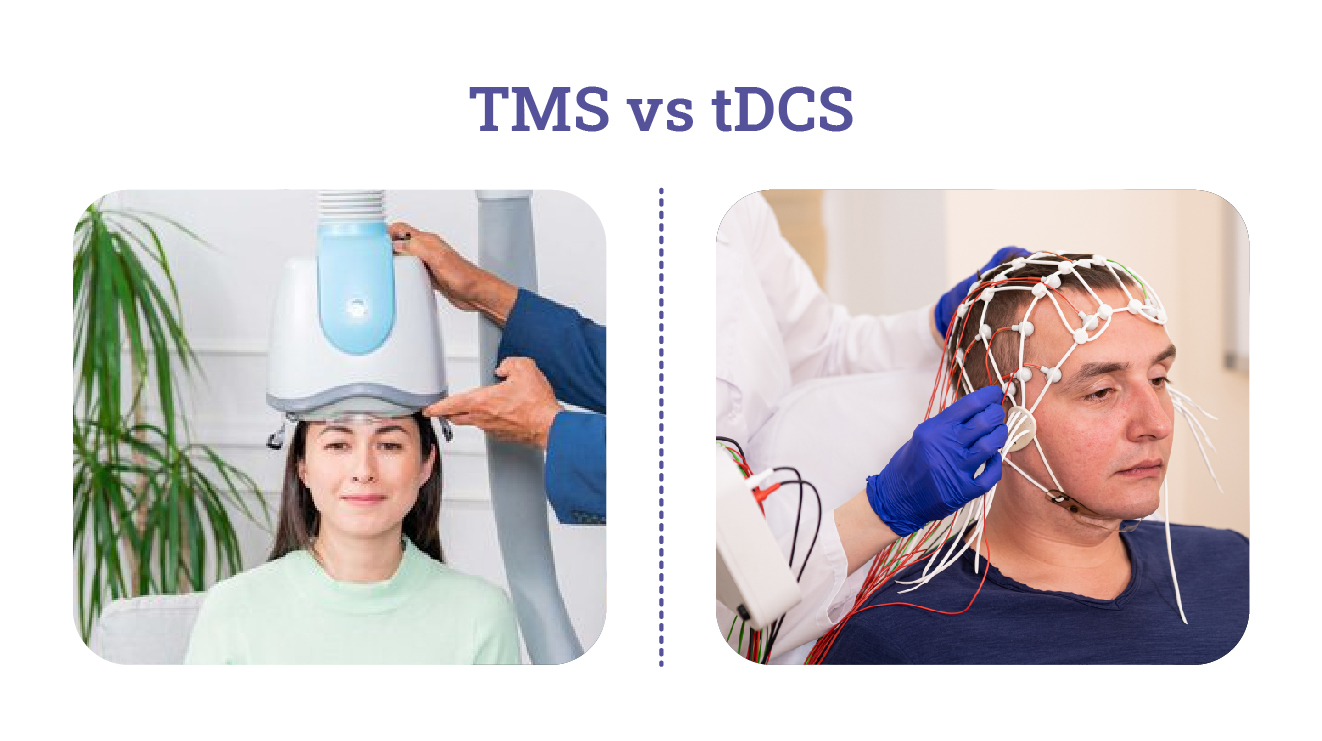
Neurostimulation—a type of therapy that uses electricity to stimulate brain activity—has gained prominence in psychiatry for its potential to treat a range of mental health conditions. Transcranial Magnetic Stimulation (TMS) and transcranial direct current stimulation (tDCS) are two kinds of non-invasive neurostimulation techniques you may see offered as a treatment for depression, obsessive-compulsive disorder (OCD), or other types of mental illnesses. Although TMS and tDCS may sound similar, there are many differences that patients should be aware of before trying one of these therapies. To help you make an informed decision on transcranial direct current stimulation vs TMS, we’ll compare these two modern neurostimulation techniques, outlining their differences in mechanisms, applications, benefits, and potential drawbacks.
Jump To:
- Transcranial Direct Current Stimulation VS TMS: What’s The Difference?
- What Is Transcranial Magnetic Stimulation (TMS)?
- What Is Transcranial Direct Current Stimulation (tDCS)?
- Difference Between TMS And tDCS
- How Do The Effects Of TMS And tDCS Differ?
- TMS VS tDCS: Clinical Studies And Evidence
- Are TMS And tDCS Treatments Covered By Insurance?
- Conclusion
Transcranial Direct Current Stimulation VS TMS: What’s The Difference?
Both kinds of neuromodulation are based on our knowledge of how the brain works, i.e., that irregularities in the brain’s electrochemical activity can cause the symptoms of mental illness. For example, a deficiency in the production of serotonin in the prefrontal cortex can cause symptoms of depression. By using electricity to stimulate the brain’s natural electrochemical activity, these therapies modulate or “fix” these irregularities and alleviate a patient’s symptoms.
The main difference when considering transcranial direct current stimulation vs TMS is the method of application. TMS utilizes a magnetic field to stimulate specific brain regions, while tDCS involves the application of low-level electrical currents directly to the scalp.
What Is Transcranial Magnetic Stimulation (TMS)?
How TMS works
TMS, first introduced in the mid-1980s, uses rapidly changing magnetic fields to induce small electrical currents in targeted brain areas. TMS is applied by a helmet-like device, known as a coil, that generates tiny, barely perceptible magnetic pulses that penetrate the skull and stimulate the neurons. By modulating neural activity, TMS can “reset” brain functions and alleviate symptoms of depression and related mental health conditions.
TMS Common Uses And Indications
TMS is primarily used in the treatment of major depressive disorder (MDD) and has received FDA approval due to the effectiveness of TMS for depression, as well as for OCD. It is also used to manage other mental health conditions, such as anxiety and post-traumatic stress disorder (PTSD).
What Is Transcranial Direct Current Stimulation (tDCS)?
How tDCS Works
tDCS, with its roots dating back to the early 19th century, involves the application of a low, direct electric current to the scalp using electrodes. tDCS works by altering the resting membrane potential of neurons and can enhance or suppress brain activity depending on the polarity of the stimulation.
tDCS Common Uses And Indications
Unlike TMS, tDCS is not FDA-approved for any specific medical use. However, it has been explored as a potential therapy for various mental health conditions, including depression, chronic pain, and cognitive enhancement (to boost memory and concentration). It is also used in research settings to investigate brain functions. Because tDCS devices are simpler and cheaper to make than TMS coils, they are often sold and marketed for home use, making them more accessible than TMS for many patients.
tDCS Benefits
The benefits of transcranial direct current stimulation vs TMS include:
- Distributed effects: tDCS affects larger brain areas, which can benefit network-level modulation. This makes tDCS suitable for studies or treatments aiming to modulate broader cognitive or motor networks, like enhancing learning or rehabilitation after a stroke.
- Gradual onset: tDCS can produce gradual, cumulative effects that are less intense but still significant over time, with a lower risk of strong side effects. This can be preferred in situations such as research for cognitive enhancement or chronic pain management.
- Portability: tDCS devices are small and portable compared to TMS devices, which make them viable for home use.
tDCS Side Effects
tDCS is relatively safe and well-tolerated. Side effects are generally mild and can include tingling sensations, itching, or mild headaches. However, it is important to note that tDCS is still largely unregulated and uncertified, and the various tDCS devices sold for home use or administered by non-physicians cannot guarantee the safety controls one would find in a clinical setting.
Difference Between TMS And tDCS
Let’s compare TMS and tDCS based on key criteria:
| Criteria | TMS | tDCS |
| Mechanism | Tiny magnetic fields to targeted brain area | Direct electrical current to scalp |
| Application | Used to treat MDD, OCD, anxiety, and PTSD | Used for research and as a potential therapy for mental health disorders |
| Duration of Treatment | Daily sessions for several weeks | Often shorter, daily, or as needed |
| Side Effects | Headache, scalp discomfort, rare seizures (less than 1%) | Mild side effects, e.g., tingling. However, devices are unregulated/uncertified and may carry risk |
| Cost | Moderate to high (average $7000 – $8000 for complete treatment). May be covered by health insurance. | Relatively low ($50-$500 for a personal device). Not covered by insurance. |
| Efficacy | Proven for some conditions, FDA-approved for MDD and OCD | Varied, more research needed |
| Contraindications | Certain medical and metal implants | Certain medical and metal implants, migraines, recent head trauma |
How Do The Effects Of TMS And tDCS Differ?
Although both TMS and tDCS are noninvasive brain stimulation methods, they affect the brain differently.. TMS directly induces neurons to fire, whereas tDCS modulates the resting membrane potential of neurons, i.e., the electrical potential difference across the neuron’s plasma membrane when the neuron is at rest. Both of these phenomena can be important in the brain’s functioning.
When considering transcranial direct current stimulation vs TMS, bear in mind that:
- The effects of TMS are usually more immediate and can last from minutes to hours after a session, depending on the protocol used. Repeated sessions can lead to longer-lasting effects, with a high success rate for treating depression and other mood disorders, making TMS useful for long-term therapeutic interventions.
- The effects of tDCS are generally more gradual, with changes in cortical excitability developing over several minutes of stimulation. Because tDCS is less targeted than TMS, effects are usually subtler and often require repeated sessions to accumulate significant changes, which can last for a few hours after stimulation. Longer-lasting effects typically require multiple sessions over days or weeks.
TMS VS tDCS: Clinical Studies And Evidence
How Do TMS And tDCS Compare In Terms Of Efficacy For Depression?
There are only a few clinical studies that have made a head-to-head comparison of TMS and tDCS for major depressive disorder (MDD). However, recent research papers have compared the results of similar studies using TMS and tDCS for depression and other mood disorders, finding that both therapies were generally effective and well-tolerated and could benefit patients when applied in different ways (1, 2). Studies have also been conducted on the combined use of TMS and tDCS for depression, with results suggesting that the two methods can complement each other for even more effective depression relief (3).
A study on tDCS for home use with remote monitoring by physicians has shown mixed results, with some groups not achieving any improvements compared to a sham treatment (4). However, more closely monitored clinical studies have shown that tDCS does appear to reduce symptoms of depression and anxiety (5). Further research using control groups and larger samples is required before a consistent, reliable method of tDCS is available for patients.
TMS, on the other hand, has a well-documented success rate of around 75% for treating MDD, with similar results for OCD (6, 7, 8). While TMS has received FDA approval for these conditions, tDCS is still in the investigational stage for many indications. Although research continues to evolve, the balance of evidence favors TMS as a safer and more effective neurostimulation therapy.
More Resources On TMS & Depression:
- What Is Depression? Causes, Symptoms, Types, And More
- TMS Therapy Success Rates For Depression And Related Conditions
- Advantages Of A Drug-Free Depression Treatment
- Deep TMS Therapy For Depression
- TMS For Seasonal Depression
- How the Brain Changes During Depression Treatment
Are TMS And tDCS Treatments Covered By Insurance?
TMS is often covered by insurance, particularly for treatment-resistant depression in patients who have not responded to other forms of treatment like medications and psychotherapy. Coverage has been expanding, and most major insurance providers, including Medicare, typically cover TMS for depression. However, the approval process can be rigorous, requiring documentation of treatment-resistant depression and often a trial of multiple antidepressants before approval.
tDCS is generally not covered by insurance for clinical use, as it is still considered an experimental or investigational treatment by many insurance companies. It is often used in research settings, and while it shows promise in various conditions like depression, chronic pain, and cognitive enhancement, it lacks the same level of regulatory approval and clinical evidence as TMS.
Conclusion
While TMS and tDCS are based on the same scientific principles, only TMS is FDA-approved and regulated for mental health treatments. As such, TMS is more widely used by doctors and recommended for individuals with treatment-resistant depression and other mood disorders.
As always, it is crucial to consult with healthcare professionals to determine the most suitable approach for your needs when it comes to any mental health condition. Madison Avenue TMS & Psychiatry offers talk therapy, medication management services, and TMS for treating depression, anxiety, and other mental health disorders. Contact us online or call (212) 731-2033 if you have any questions or to make an appointment.
Learn More About Neurostimulation Therapies:
- Deep Brain Stimulation VS TMS
- TMS Therapy VS ECT: What’s The Difference?
- Bilateral TMS Treatment vs Unilateral TMS Treatment
Sources:
- Hejzlar, M., Novak, T., & Bares, M. Neurostimulation Methods in the Treatment of Depression: A Comparison of rTMS, tDCS, and Venlafaxine Using a Pooled Analysis of Two Studies. Neuropsychiatric Disease and Treatment. 2021;17, 1713-1722. Link. Accessed August 27, 2024.
- Sabé M, Hyde J, Cramer C, et al. Transcranial Magnetic Stimulation and Transcranial Direct Current Stimulation Across Mental Disorders: A Systematic Review and Dose-Response Meta-Analysis. JAMA Netw Open. 2024;7(5):e2412616. Link. Accessed August 27, 2024.
- Li, X., Liu, J., Wei, S. et al. Cognitive enhancing effect of rTMS combined with tDCS in patients with major depressive disorder: a double-blind, randomized, sham-controlled study. BMC Med. 2024;22, 253. Link. Accessed August 27, 2024.
- Borrione L, Cavendish BA, Aparicio LVM, et al. Home-Use Transcranial Direct Current Stimulation for the Treatment of a Major Depressive Episode: A Randomized Clinical Trial. JAMA Psychiatry. 2024;81(4):329–337. Link. Accessed August 27, 2024.
- Zheng, E. Z., Wong, N. M., Yang, A. S., & Lee, T. M. (2024). Evaluating the effects of tDCS on depressive and anxiety symptoms from a transdiagnostic perspective: A systematic review and meta-analysis of randomized controlled trials. Translational Psychiatry, 14(1), 1-15. Link. Accessed August 27, 2024.
- Bouaziz, N., Laidi, C., Bulteau, S., Berjamin, C., Thomas, F., Moulier, V., Benadhira, R., Szekely, D., Poulet, E., Galvao, F., Guillin, O., Castillo, M., Sauvaget, A., Plaze, M., Januel, D., Brunelin, J., & Rotharmel, M. Real world transcranial magnetic stimulation for major depression: A multisite, naturalistic, retrospective study. Journal of Affective Disorders. 2023;326, 26-35. Link. Accessed August 27, 2024.
- Tendler, A., Goerigk, S., Zibman, S., Ouaknine, S., Harmelech, T., Pell, G. S., Zangen, A., Harvey, S. A., Grammer, G., Stehberg, J., Adefolarin, O., Muir, O., MacMillan, C., Ghelber, D., Duffy, W., Mania, I., Faruqui, Z., Munasifi, F., Antin, T., . . . Roth, Y. Deep TMS H1 Coil treatment for depression: Results from a large post marketing data analysis. Psychiatry Research. 2023;324, 115179. Link. Accessed August 27, 2024.
- Vinod, P., Thatikonda, N. S., Malo, P. K., Bhaskarapillai, B., Arumugham, S. S., & Janardhan Reddy, Y. (2024). Comparative efficacy of repetitive transcranial magnetic stimulation protocols for obsessive-compulsive disorder: A network meta-analysis. Asian Journal of Psychiatry, 94, 103962. Link. Accessed August 27, 2024.
Dr. David Woo is the owner and head clinical psychiatrist at Madison Avenue TMS and Therapy in New York City. Dr. Woo has been seeing patients in private practice since 2002, always with the goals of combining evidence-based medicine with psychodynamic psychotherapy and collaborating with other mental health professionals to ensure the best possible outcomes for his patients. He has been certified to administer TMS at his practice since 2017. His greatest clinical interests include helping patients suffering from depression, anxiety, and obsessive compulsive disorder.
Follow Dr. Woo On
Dr. Woo On The Web



