What do you think of this article?
By Dr. David Woo - September 18, 2023
Published on September 18, 2023 … Updated on April 30, 2024
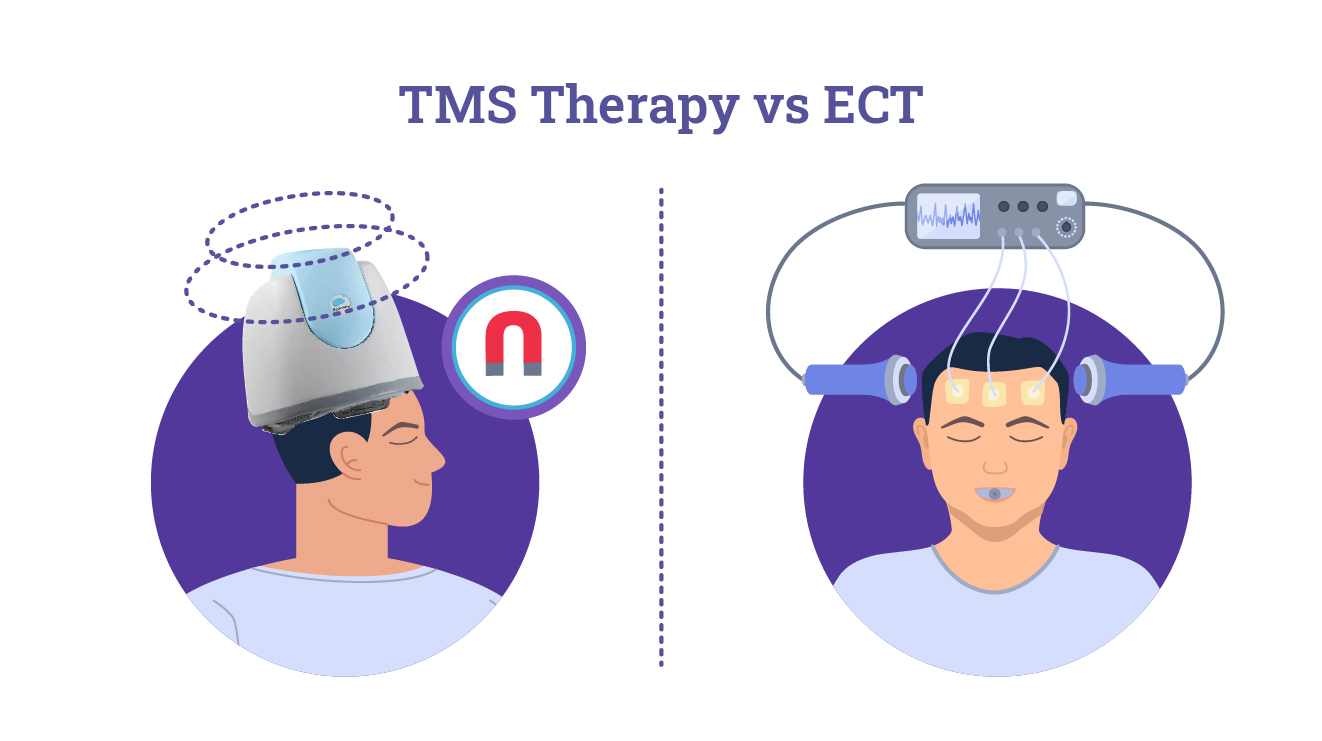
Transcranial magnetic stimulation (TMS) and electroconvulsive therapy (ECT) are two different mental health therapies that have garnered attention for their effectiveness in treating mood disorders, especially major depressive disorder (MDD). Because both therapies use electric pulses to activate the natural electro-chemical activity of the brain, they often invite comparison and can sometimes be confused with each other. Nonetheless, TMS and ECT are completely different procedures in terms of their mechanisms, side effects, and applications.
Is TMS or ECT right for you? This article looks at TMS therapy versus ECT and answers some common questions about the benefits and drawbacks of each.
Jump to:
- What’s The Difference Between TMS And ECT?
- TMS vs. ECT Comparison Table
- Why Is ECT A Last Resort?
- Why You Might Hear “ECT Ruined My Life”
- ECT vs. TMS For Depression: Is ECT More Effective Than TMS?
- What Is One Serious Drawback Of ECT?
- Does ECT Make Anxiety Worse?
- When Should ECT Not Be Used?
- How Much Does TMS Cost Compared To ECT?
- Why Choose TMS Over ECT?
What’s The Difference Between TMS And ECT?
TMS therapy employs repetitive magnetic pulses to the brain area associated with mood disorders, e.g., the prefrontal cortex in the case of depression. The pulses stimulate the activity of the neurons inside the brain in a way that can alleviate a patient’s symptoms. TMS is noninvasive and administered via a head-mounted device similar to a bathing cap. This therapy is FDA-approved for cases of depression and obsessive-compulsive disorder (OCD) in cases where pharmaceuticals have proven ineffective (1). Still, research has also shown it to have positive effects in treating anxiety, attention-deficit hyperactivity disorder (ADHD), and borderline personality disorder (BPD).
ECT, often called “shock therapy,” is a more intense treatment that is used as a last resort. ECT aims to rewire brain circuits by inducing controlled seizures by applying electric currents to the brain. It is used to treat especially severe depression, bipolar disorder, and schizophrenia, typically in emergencies or life-threatening cases.
TMS vs. ECT Comparison Table
| Therapy | TMS | ECT |
| Procedure | Noninvasive (helmet-like device on the scalp sends gentle electromagnetic pulses to targeted brain regions) | Invasive (incision made to pass electric currents through the brain to induce controlled seizures) |
| Anesthesia | Not required | Generally required |
| Side effects | Mild to none, can include headache, scalp discomfort, muscle twitching, and in rare cases, seizures | More severe, including short-term memory loss, confusion, headaches, and muscle aches |
| Treatment course | Typically 4-6 weeks of daily sessions, each lasting 20-40 minutes | Rapid improvement often noticed after just a few sessions |
| Maintenance | May require occasional TMS maintenance sessions or booster treatments to sustain benefits | May require maintenance treatments over time to prevent relapse |
| Cost | Varies, averages around $500 per session, but is covered by many insurance plans | Varies, averages around $2500 per session |
Why Is ECT A Last Resort?
ECT requires anesthesia and muscle relaxants to prevent bodily harm during seizures. Another primary concern surrounding ECT is its potential for cognitive side effects, such as memory loss and confusion, which can sometimes be significant (2). Because of these factors and the existence of less severe noninvasive alternatives such as TMS, ECT is generally recommended as a last resort or second-line treatment unless rapid emergency intervention is necessary (for example, a threat of imminent harm or suicide).
Furthermore, ECT is an inpatient procedure that requires hospitalization and the support of family members, friends, or caregivers to provide transportation and care before and after treatment.
Why You Might Hear “ECT Ruined My Life”
ECT’s potential cognitive side effects include memory loss, specifically retrograde amnesia (difficulty recalling past events) and anterograde amnesia (difficulty forming new memories). This can disrupt personal, professional, and social affairs, making it more difficult for the depressed patient to reintegrate into a regular, healthy routine.
Because of these disruptive side effects, you may hear negative testimonies from ECT patients. Ultimately, the decision to undergo ECT must not be taken lightly, and it remains a second-line treatment for use in emergencies or after alternatives have been exhausted.
ECT vs TMS For Depression: Is ECT More Effective Than TMS?
ECT’s effectiveness is often acknowledged, especially in cases of severe depression where rapid intervention is necessary. In one study of TMS versus ECT for patients with MDD, ECT outperformed TMS on the Hamilton Rating Scale for Depression, reducing symptoms by 15 points as opposed to 9 points for TMS (3). However, the TMS success rate for alleviating symptoms of depression is excellent, and the advantages of TMS in terms of safety, convenience, and long-term prospects make it a preferable first option for many patients with treatment-resistant depression.
What Is One Serious Drawback Of Using ECT To Treat Depression?
As well as the potential cognitive side-effects, it should be noted that remission from ECT is often short-term and that in the long term, most patients will require antidepressant medications to manage their symptoms. Antidepressants are not always effective and come with their own side effects, and TMS is a recommended treatment for patients who wish to avoid or reduce dependency on antidepressant drugs.
Does ECT Make Anxiety Worse?
While the procedure of ECT does not itself cause anxiety, patients with anxiety can experience heightened anxiety and excessive worry centered around the potential side effects of ECT. ECT-related anxiety is a documented phenomenon and sometimes requires additional medical intervention in the form of anti-anxiety medications (4).
When Should ECT Not Be Used?
Given the potential risks involved, ECT should not be used if you have:
- Mild or moderate depression
- Certain cardiovascular conditions, such as heart attacks, severe hypertension, recent heart attacks or strokes
- A history of adverse reactions to anesthesia
- Certain neurological conditions, such as brain tumors or recent head injuries
In all cases, a thorough evaluation of the patient’s condition and the clinical necessity of the treatment should be conducted before ECT is applied.
Which Is Safer, ECT Or TMS?
Unlike ECT, TMS does not induce seizures or require anesthesia or hospitalization, making it less risky and more patient-friendly. Additionally, TMS has fewer cognitive side effects at a much lower risk, meaning patients can often return to their daily activities immediately after a session.
The precisely targeted nature of TMS means that it will not affect other bodily systems. Although some TMS patients report a mild headache or scalp irritation after a session, these can be easily treated with over-the-counter medications.
How Much Does TMS Cost Compared To ECT?
TMS therapy costs tend to be overall less expensive than ECT, as it requires no hospital time and demands fewer resources from medical providers. Although prices vary according to location and a patient’s needs, the average ECT session costs about $2500 compared to a $400-$500 session of TMS. In many cases, TMS is covered by insurance and Medicare, as is ECT, but it is important to check if TMS is covered by insurance under your specific provider first.
Why Choose TMS Over ECT?
Unless one’s condition is especially severe or life-threatening, most patients prefer TMS over ECT due to its noninvasive nature, cost-effectiveness, and minimal disruption to daily life (5).
Madison Avenue TMS & Psychiatry offers talk therapy and TMS for treating depression, anxiety, and other mental health conditions. Contact us online or call (212) 731-2033 for more information or to make an appointment.
More resources on TMS vs. alternative therapies:
- dTMS vs. rTMS: What’s The Difference?
- Ketamine vs. TMS: Which One Is Right For You?
- TMS Therapy vs. Deep Brain Stimulation: What’s The Difference?
Resources:
- FDA permits marketing of transcranial magnetic stimulation for treatment of obsessive compulsive disorder. U.S. Food & Drug Administration. Updated August 17, 2018. Link. Accessed July 17, 2023.
- Porter, R., Baune, B., Morris, G., Hamilton, A., Bassett, D., Boyce, P., . . . Malhi, G. Cognitive side-effects of electroconvulsive therapy: What are they, how to monitor them and what to tell patients. BJPsych Open. 2020;6(3). Link. Accessed August 14, 2023.
- Micallef-Trigona. Comparing the effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in the treatment of depression: a systematic review and meta-analysis. Depression Research and Treatment. 2014. Link. Accessed August 14, 2023.
- Obbels J, Verwijk E, Bouckaert F, Sienaert P. ECT-Related Anxiety: A Systematic Review. J ECT. 2017;33(4):229-236. Link. Accessed April 27, 2024.
- Magnezi R, Aminov E, Shmuel D, Dreifuss M, Dannon P. Comparison between neurostimulation techniques repetitive transcranial magnetic stimulation vs electroconvulsive therapy for the treatment of resistant depression: patient preference and cost-effectiveness. Patient Prefer Adherence. 2016;10:1481-7. Link. August 14, 2023.
Dr. David Woo is the owner and head clinical psychiatrist at Madison Avenue TMS and Therapy in New York City. Dr. Woo has been seeing patients in private practice since 2002, always with the goals of combining evidence-based medicine with psychodynamic psychotherapy and collaborating with other mental health professionals to ensure the best possible outcomes for his patients. He has been certified to administer TMS at his practice since 2017. His greatest clinical interests include helping patients suffering from depression, anxiety, and obsessive compulsive disorder.
Follow Dr. Woo On









