What do you think of this article?
By Dr. David Woo - September 25, 2023

Published: September 25, 2023 Updated: September 18, 2024
The field of mental health treatment is constantly evolving and adopting new therapies based on emerging research and evidence. In this article, we will compare two therapies that are gaining in popularity as alternative treatments for depression and other mood disorders: ketamine and transcranial magnetic therapy (TMS). Both of these innovative treatments are effective for depression, but each has its pros and cons. If you’re weighing up whether TMS or ketamine might be right for you, read on to discover the relative benefits of TMS vs ketamine.
Jump to:
- TMS VS Ketamine: A Side-By-Side Comparison
- Ketamine Therapy VS TMS Comparative Table
- Ketamine Therapy VS TMS: How Do They Work?
- What Conditions Are Treated With Ketamine And TMS?
- How Long Is Each Treatment, And How Quickly Can Patients See Results From Ketamine VS TMS?
- Are Ketamine And TMS Covered By Insurance?
- How Do The Costs Of Ketamine And TMS Treatments Compare?
- How Effective Is Ketamine Compared To TMS For Treating Depression?
- Are There Any Long-Term Risks Associated With Ketamine Or TMS?
- Who Is A Good Candidate For Ketamine Treatment VS TMS?
- Can Ketamine And TMS Be Used Together In Treatment Plans?
TMS VS Ketamine: A Side-By-Side Comparison
TMS and ketamine are very distinct forms of therapy, even if they can be used to treat the same conditions. They differ greatly in terms of application, onset, insurance coverage, and many other factors. Let’s look at the pros and cons of Ketamine vs TMS.
Ketamine Therapy VS TMS Comparative Table
| Category | Ketamine Therapy | TMS (Transcranial Magnetic Stimulation) |
| Mechanism of Action | Targets the brain’s glutamate receptors to promote synaptic plasticity and new neural connections. | Uses electromagnetic fields to stimulate specific brain areas, promoting neuroplasticity and new connections. |
| Application | As a nasal spray (esketamine) or an IV drip (as an anesthetic). | Noninvasive application via a helmet-like device with an electromagnetic coil. |
| Conditions Treated | Nasal spray is FDA-approved for treatment-resistant depression and suicidal thoughts (nasal spray); also shows promise for anxiety and PTSD. Off-label use of IV ketamine for depression. | FDA-approved for major depressive disorder (MDD) and obsessive-compulsive disorder (OCD); also effective for anxiety, bipolar disorder, borderline personality disorder (BPD), PTSD, and eating disorders. |
| Onset of Effectiveness | Rapid onset; relief often within hours or days. | Positive results typically seen after several sessions; longer-lasting effects compared to ketamine. |
| Duration of Treatment | Nasal spray application followed by a two-hour monitoring period; administered twice weekly initially, with tapering over time. | Average course consists of around 30 sessions, each lasting about 30 minutes. |
| FDA Approval | Esketamine nasal spray is FDA-approved; IV ketamine is approved as an anesthetic (off-label for mental health). | FDA-approved for MDD and OCD. |
| Insurance Coverage | Generally not covered by insurance; esketamine nasal spray may be covered by some plans. | Covered by many private insurance plans and Medicare. |
| Cost | Approximately $400 per session; long-term treatment may cost thousands due to the need for frequent sessions. | Full 9-week course ranges from $7,000 to $15,000; insurance may cover a significant portion, reducing out-of-pocket costs. |
| Pros | Fast-acting; effective in reducing suicidal ideation; useful in acute crisis situations. | Drug-free; long-lasting effects, noninvasive with minimal side effects. |
| Cons | Short-lived effects, high relapse rate, lack of standardization in treatment, potential side effects (disorientation, hallucinations, cardiovascular and urinary issues), risk of abuse. | Requires multiple sessions, slower onset, 1% chane of seizures. |
| Long-Term Risks | Potential cognitive impairment at high doses, though not typically seen at clinical doses. | Generally well-tolerated; mild side effects like scalp irritation or headache; rare risk of seizures. |
| Best Suited For | Acute and severe depression, especially when symptoms are threatening immediate health and safety. | Mild to moderate, long-lasting depression; suitable for those seeking non-medication treatment or with contraindications for ketamine. |
Ketamine Therapy VS TMS: How Do They Work?
Ketamine
Ketamine was initially developed as an anesthetic and gained notoriety as a recreational substance. However, it has been recognized by the medical establishment as a rapid-acting antidepressant and anxiolytic (anti-anxiety) agent (1). This is because the drug targets the brain’s glutamate receptors, promoting synaptic plasticity, which enhances the formation of new neural connections to regulate brain activity. Ketamine is typically applied in a controlled clinical setting as an intravenous (IV) drip or as a nasal spray (esketamine).
TMS
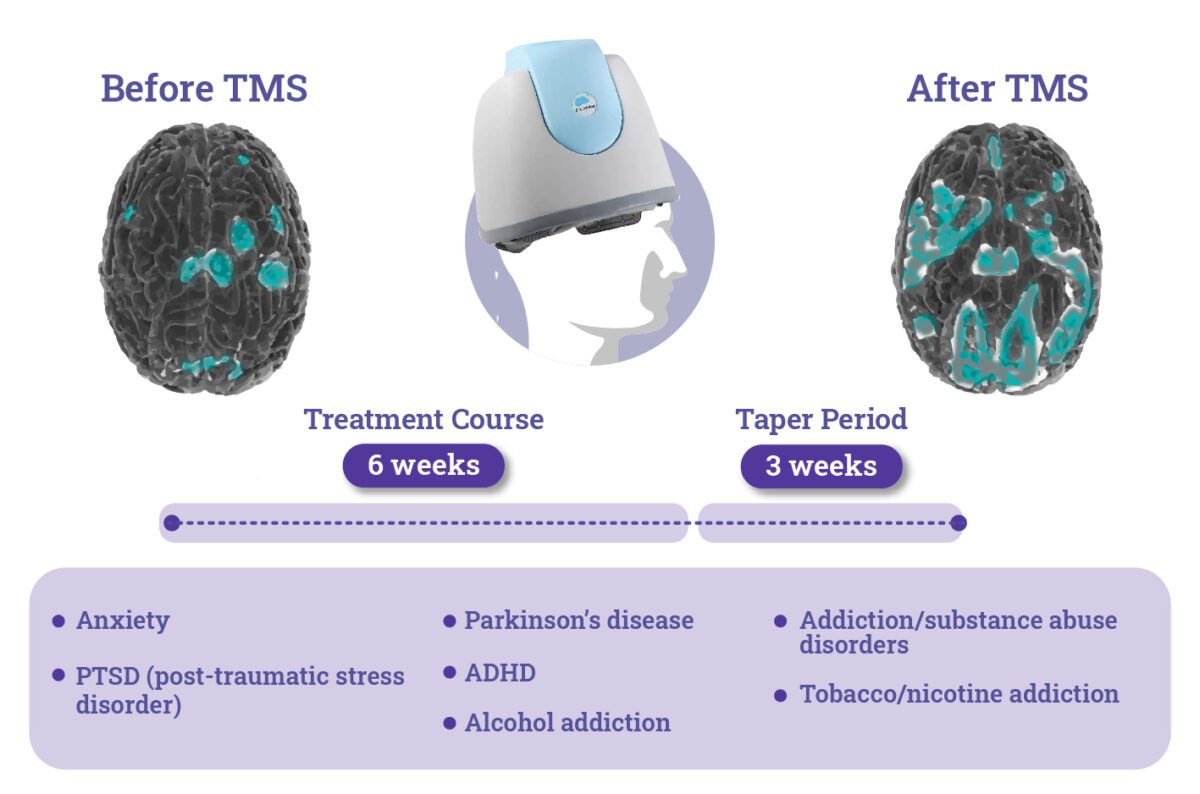
Transcranial Magnetic Stimulation (TMS) is a noninvasive procedure that uses a helmet-like device to deliver tiny, barely perceptible electromagnetic fields through the scalp in order to stimulate specific brain areas associated with the patient’s symptoms. By modulating the brain’s natural electrochemistry, it promotes neuroplasticity and new connections in the targeted brain area and has been shown to be effective in relieving symptoms of depression (2).
What Conditions Are Treated With Ketamine And TMS?
Both TMS and ketamine are increasingly popular alternative therapies for treatment-resistant depression, i.e., in cases where at least two different antidepressants have failed to alleviate a patient’s symptoms satisfactorily.
If you are on medication for depression, anxiety, or another mood disorder and feel like the drugs aren’t working, then it’s important to consult with a mental health professional to check your progress and explore alternatives. Madison Avenue TMS & Psychiatry offers medication management services via telehealth consultations to ensure patients’ medications are working for them and to see if alternatives such as TMS or ketamine may be worth trying.
TMS therapy is FDA-approved for:
- Major depressive disorder (MDD), which is its primary application
- Obsessive-compulsive disorder (OCD) (3)
- Anxious depression
TMS has also been shown to be effective in treating other mood disorders, such as:
- Anxiety
- Bipolar disorder
- Borderline personality disorder (BPD)
- Post-traumatic stress disorder (PTSD)
- Eating disorders
The esketamine nasal spray is used to treat:
IV ketamine is only approved as an anesthetic, and its use for mental health disorders is considered an “off-label,” unofficial application.
How Long Is Each Treatment?
Typical ketamine treatment involves an application of the nasal spray, followed by a two-hour monitoring period. After that, the dosage is maintained twice weekly for the first month to reduce dosage and taper off over time.
On the other hand, the average course of TMS consists of around thirty sessions, each around thirty minutes long.
How Quickly Can Patients See Results From Ketamine VS TMS?
One of the most significant advantages of ketamine is its rapid onset time. Many patients experience relief from depressive symptoms within hours or days, compared to the weeks typically required for traditional antidepressant medications.
When it comes to TMS, patients typically report positive results after several sessions rather than immediately. However, the effects of TMS appear to last longer than ketamine, making it less effective in emergencies but more effective for long-term relief.
Are Ketamine And TMS Covered By Insurance?
When considering the cost of TMS vs ketamine therapy, it’s important to bear in mind that ketamine as a depression treatment is still relatively new, and as such, is very unlikely to be covered by insurance. However, as the use of the esketamine nasal spray in a clinical setting is becoming more widespread, it is worth checking with your insurance company.
TMS is a more established therapy that is covered by many private insurance plans and Medicare.
How Do The Costs Of Ketamine And TMS Treatments Compare?
When comparing the costs of ketamine therapy and TMS, ketamine infusions typically start around $400 per session, with long-term treatment potentially costing thousands of dollars, as ketamine is associated with a high rate of relapse, so multiple sessions are often required.
In contrast, a full 9-week course of TMS treatment usually ranges from $7,000 to $15,000, depending on the equipment used, the practitioner, the location, and any need for an extension of treatment. However, insurance may cover a significant portion if specific criteria are met. Overall, TMS costs more than ketamine up front if uninsured, but insurance coverage can reduce out-of-pocket expenses compared to ketamine therapy, and its results are proven to be longer lasting.
At Madison Avenue TMS & Psychiatry, our mission is to make TMS accessible to everyone who needs it, and we work with insured and uninsured patients alike to keep their TMS costs affordable. If you’re in need of help but worried about the financial burden, please contact us to see what we can do for you.
How Effective Is Ketamine Compared To TMS For Treating Depression?
TMS and Ketamine are both effective therapies for treatment-resistant depression. However, each is most suited to different circumstances.
The advantages of ketamine as a depression treatment are that it is:
- Fast-acting – The drug’s rapid onset can provide swift relief. This makes it most effective in urgent crisis situations when it can serve as a bridge between the emergency response and a long-term treatment plan
- Effective in reducing suicidal ideation – Research has shown ketamine reduces suicidal thoughts in patients.
However, longer studies into ketamine’s effectiveness have shown a high chance of relapse, e.g., only a 15% remission rate after 6 months of ketamine administration (5).
TMS therapy’s success rate for depression is more well-documented, with the following advantages compared to ketamine:
- Drug-free depression treatment – TMS doesn’t involve any pharmaceutical interventions and therefore is attractive to individuals who are concerned about drug interactions and side effects.
- TMS has been proven effective in the long term – Patients who struggle with depression for extended periods may prefer TMS, with its documented long-lasting effects.
Are There Any Long-Term Risks Associated With Ketamine Or TMS?
TMS Therapy Side Effects
TMS is safe and generally well-tolerated, with most patients experiencing no side effects. A minority of TMS patients report mild side effects, such as light scalp irritation or headache, which are easily treatable with over-the-counter medications.
However, in a small minority of cases, TMS has been known to cause seizures. As such, it should only be conducted in a clinic by a qualified professional.
“Ketamine Ruined My Life” – What Are The Risks?
Despite its advantages as a fast-acting depression treatment, ketamine does have some drawbacks, including:
- Short-lived effect – The effects of ketamine are often temporary, necessitating frequent administrations to sustain positive outcomes. This can pose challenges in terms of logistics, costs, and potential side effects.
- Lack of standardization – There is still a lack of consensus on optimal dosing, frequency, and duration of ketamine treatments. This variability can affect treatment outcomes and patient safety.
- Side effects – Common side effects of ketamine include disorientation, hallucinations, and potential cardiovascular and urinary issues (6).
- Risk of abuse – Ketamine has a history of recreational misuse due to its dissociative properties. Its potential for abuse raises concerns, particularly when administered outside of controlled medical environments.
The risks of ketamine, and its status as a popular recreational drug, mean that ketamine therapy for mental health issues is strictly controlled and being rolled out carefully into the wider healthcare system. In the long term, ketamine at high doses is known to impair cognitive function, although this has not been found to be the case for clinically administered doses for depression treatment (7).
Who Is A Good Candidate For Ketamine Treatment VS TMS?
In all cases, treatment decisions for mental health conditions should be taken in consultation with a qualified mental health professional. However, generally speaking, if traditional medications and psychotherapy haven’t relieved your symptoms or if you experience unpleasant side effects from antidepressants, then it may be time to consider alternatives such as ketamine or TMS.
- You might be a good candidate for ketamine therapy if your depression is acute and severe and if you are experiencing symptoms that are threatening your immediate health and safety. Ketamine’s rapid onset makes it optimally suited for quick relief.
- You might be a good candidate for TMS if your depression is mild to moderate and long-lasting or if you’re planning to become pregnant and need a non-medication treatment for depression. Additionally, TMS is suitable for those without a history of seizures or seizure disorders and without any neural implants.
Can Ketamine And TMS Be Used Together In Treatment Plans?
With your doctor’s approval it may be possible to combine both therapies. Research has shown that both treatments can be used together and appear to complement each other in stimulating the brain to alleviate depression symptoms, while there does not appear to be any additional risk in combined therapy (8). However, the testing of this combination therapy is still in its early stages.
Struggling with depression in NYC? Is your medication not working for you? Don’t hesitate to seek help—there are many treatments to combat depression, and you should explore all the options.
Madison Avenue TMS & Psychiatry offers talk therapy, medication management services, and innovative therapies like TMS for depression and other mental health conditions. Contact us online or call (212) 731-2033 for more information or to make an appointment.
Discover More Innovative Depression Treatments:
- Lithium For Depression
- TMS And Psychedelics
- Deep Brain Stimulation VS TMS
- TMS VS tDCS: A Deep Dive
- TMS Therapy VS ECT: What’s The Difference?
Sources:
- Andrade C. Ketamine for Depression—Knowns, Unknowns, Possibilities, Barriers, and Opportunities. JAMA Psychiatry. 2023;80(12):1189–1190. Link. Accessed August 26, 2024.
- Moro, A. S., Saccenti, D., Vergallito, A., Gregori Grgič, R., Grazioli, S., Pretti, N., Crespi, S., Malgaroli, A., Scaini, S., Ruggiero, G. M., Sassaroli, S., Ferro, M., & Lamanna, J. Evaluating the Efficacy of Transcranial Magnetic Stimulation in Symptom Relief and Cognitive Function in Obsessive–Compulsive Disorder, Substance Use Disorder, and Depression: An Insight from a Naturalistic Observational Study. Applied Sciences. 2023;14(14), 6178. Link. Accessed August 26, 2024.
- FDA permits marketing of transcranial magnetic stimulation for treatment of obsessive compulsive disorder. U.S. Food & Drug Administration. Updated August 17, 2018. Link. Accessed August 16, 2023.
- FDA approves new nasal spray medication for treatment-resistant depression; available only at a certified doctor’s office or clinic. U.S. Food & Drug Administration. Updated March 05, 2019. Link. Accessed August 16, 2023.
- Pfeiffer, P. N., Geller, J., Ganoczy, D., Jagusch, J., Carty, J., Festin, F. E. D., Gilmer, W. S., Martis, B., Ranganathan, M., Wiechers, I. R., & Hosanagar, A. Clinical outcomes of intravenous ketamine for depression in the VA health system. The Journal of Clinical Psychiatry. 2024;85(1). Link. Accessed August 26, 2024.
- Yang X, Chen D. Comparing the adverse effects of ketamine and esketamine between genders using FAERS data. Front Pharmacol. 2024;12;15. Link. Accessed August 26, 2024.
- Nikayin S, Murphy E, Krystal JH, Wilkinson ST. Long-term safety of ketamine and esketamine in treatment of depression. Expert Opin Drug Saf. 2022;21(6):777-787. Link. Accessed August 26, 2024.
- Dębowska, W., Więdłocha, M., Dębowska, M., Kownacka, Z., Marcinowicz, P., & Szulc, A. Transcranial magnetic stimulation and ketamine: Implications for combined treatment in depression. Frontiers in Neuroscience. 2023;17. Link. Accessed August 26, 2024.
Dr. David Woo is the owner and head clinical psychiatrist at Madison Avenue TMS and Therapy in New York City. Dr. Woo has been seeing patients in private practice since 2002, always with the goals of combining evidence-based medicine with psychodynamic psychotherapy and collaborating with other mental health professionals to ensure the best possible outcomes for his patients. He has been certified to administer TMS at his practice since 2017. His greatest clinical interests include helping patients suffering from depression, anxiety, and obsessive compulsive disorder.
Follow Dr. Woo On









